TREATMENT FOR CHILDREN, TEENS & ADULTS
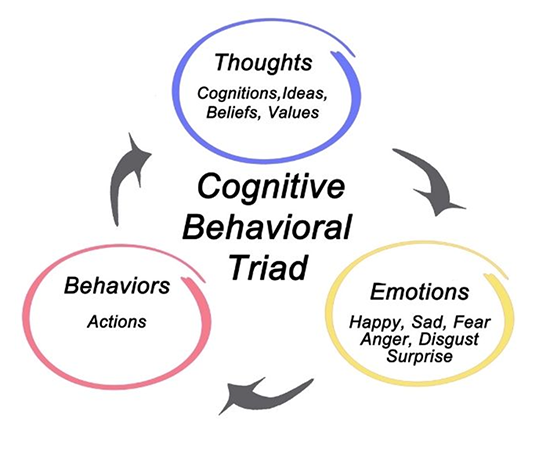
COGNITIVE-BEHAVIORAL THERAPY
We Are Accepting New Clients
Call our counseling center for a 15-Minute complimentary
phone consultation at 707-545-4600
What is Cognitive-Behavioral Therapy?
Collaborative
The client and therapist work together to understand the problem, define goals and develop the best treatment plan.
Active
During sessions as well as between sessions the client is practicing skills and for anxiety facing their fears and gaining mastery over them.
Objective
Questionnaires are used on a regular basis to monitor improvement of symptoms.
Effective
Clients usually experience meaningful lasting change in a relatively few number of sessions
![]()
CHILD THERAPY
“We believe that parents are a key part of helping children overcome their anxiety. As a result, your child’s therapist will meet with your child by themselves, you and your child together, as well as with you by yourself to make sure that you all have the tools needed to overcome their current worries and any fears or worries that may pop up in the future.”
![]()
TEEN THERAPY
Because teens are at the developmental stage of creating independence and autonomy, therapy sessions are most often conducted one-on-one with the teen. However, we still believe that parents of teens play an important role in supporting the therapeutic process.
![]()
ADULT THERAPY
Cognitive Behavioral Therapy (CBT) is a time limited goal-oriented approach to therapy that is best suited for people who have a specific problem and are looking for help to develop specific tools and strategies to overcome this problem.
Our Expertise
Panic Disorders and Agoraphobia
If you experience intense, seemingly out of the blue panic attacks and are now worried about having more, you may be struggling with Panic Disorder. The three most common fears expressed by people who have panic disorder are:
- fear of dying
- fear of going crazy
- fear of losing control
Panic attacks occur unexpectedly and can even occur during sleep.
A panic attack is a sudden and intense fear or discomfort which reaches it’s peak within 10 minutes and can include the following symptoms:
- pounding heart, palpitations, or accelerated heart rate
- sweating
- trembling or shaking
- sensations of shortness of breath or smothering
- feelings of choking
- chest pain or discomfort
- nausea or abdominal distress
- feeling dizzy, unsteady, lightheaded, or faint
- derealization (feelings of unreality) or depersonalization (being detached from oneself)
- fear of losing control or going crazy
- fear of dying
- numbness or tingling sensations
- chills or hot flushes
Many of the symptoms of panic attacks can look like those of physical illnesses such as heart disease, breathing and thyroid problems. Because of this, people who have panic attacks often go to the emergency room because they think they are suffering from a life-threatening illness. If you have experienced regular panic attacks, it is important to rule out illness that may cause panic like symptoms.
Agoraphobia
A common misconception is that agoraphobia is the fear of leaving ones home. Although people with agoraphobia sometimes become housebound due the intensity of their fears, this is not true for all people with Agoraphobia. When a person avoids places or situations from which escape might be difficult or embarrassing, or if help might be unavailable if they have a panic attack, they are agoraphobic. About one out of three people who have panic disorder develop agoraphobia.
Common avoided situations include:
- crowds
- standing in line
- bridges
- traveling in a bus, train, boat or car
To cope with their fears, specific routes or means of travel are identified as safe and any thing outside of this causes significant anxiety.
When people have agoraphobia, their world becomes smaller and smaller.
Treatment
Cognitive behavioral therapy is a highly effective treatment that can reduce the occurrence of panic attacks as well as help people feel less fearful when experiencing panic symptoms.
Social Phobia / Social Anxiety
Do you avoid social or performance situations for fear that you will say or doing something that will be humiliating or embarrassing?
Social anxiety is a fear of being scrutinized or negatively judged by others in a social or performance situation. People with social anxiety are terrified of saying or doing something that will humiliate or embarrass them. It usually starts in childhood and adolescence and continues into adulthood. It is the most common anxiety disorder.
Typical situations that cause anxiety are:
- Starting or maintaining a conversation
- Appearing nervous to others or being observed blushing, sweating or shaking.
- Using a public restroom
- Participating in small groups
- Eating in front of others
- Giving a presentation
- Asking someone out
- Being observed by others
- Being the center of attention
For children and teens, additional situations that cause anxiety are:
- Answering questions in class
- Asking the teacher a question
- Having a school picture taken
- PE
- Writing on a white board
- Inviting others to get together
People with social anxiety usually know that their anxiety is somewhat unreasonable but this does not change their reaction to situations. They often avoid the situations that make them anxious or endure it with significant distress. Common physical symptoms associated with social anxiety are blushing; sweating; shaking; nausea; rapid heartbeat; shortness of breath; dizziness; headaches. In children social anxiety can be associated with selective mutism and school refusal.
Generalized Anxiety Disorder
Do you feel consumed by your worries? Do you find that you worry about a wide range of issues such as:
- work
- school
- money
- relationships
- natural disasters
- your own or your loved one’s health
Everyone worries, but people with generalized anxiety disorder (GAD) take worry to the next level of catastrophizing, often thinking of the worst possible outcome to any situation. If their friend or mate is late they think they have been in a car accident. When there is a bad storm, they imagine trees falling on their house. When their child is sick, they imagine leukemia or some other life threatening illness.
Common symptoms that people with GAD experience are:
- Feeling tense, restless, and keyed up
- Being easily fatigued
- Difficulty concentrating
- Irritability
- Muscle tension
- Sleep disturbance – difficulty falling asleep, staying asleep, or restless unsatisfying sleep
Children also suffer from GAD. Their worries may center around their family getting sick or dying. Any bad news they hear on the TV they assume will affect them. They worry about grades or being late to school or getting sent to the principal’s office.
Treatment
Cognitive-behavior therapy can help people to think more realistically about their worries, learn to problem solve productively, accept uncertainty and feel more relaxed.
Phobias
If your fears of specific objects or situations have become extreme or unreasonable and are interfering in your daily life, you may have developed a specific phobia.
Phobias can include fears of:
- Flying
- Heights
- Water
- Animals/Insects
- Needles/Doctors/Blood
- Vomiting
- Costumed Characters
Although many people have fears of these things, a phobia develops when the fear starts to cause problems in your daily life. For example someone with a spider phobia may stop using a specific bathroom in the house after seeing a spider in the bathtub. Over time they may even avoid using any bathroom in the house without another family member checking it first to make sure there are no spiders. Like many of the other anxiety disorders, people with specific phobias also know that their fears are somewhat unreasonable. This realization however generally does not do much to reduce their anxiety in the feared situation. Because of this, many people feel embarrassed by their unreasonable fear and avoid telling people outside their family.
Treatment
Cognitive-Behavioral Therapy (CBT) helps people to face their fears in a gradual and supportive way. CBT is one of the most effective treatments for phobias, most people report feeling significantly less fearful after only 12 sessions or less.
Obsessive-Compulsive Disorder
OCD is characterized by obsessions and compulsions. Obsessions are intrusive thoughts, images, or impulses that are unwanted or inappropriate and appear to be outside of a person’s control. Obsessions tend to cause significant stress and anxiety because the content of the thoughts are often in direct opposition to how the person typically thinks or feels. Often the person recognizes that the thoughts are irrational or bizarre, but is unable to be fully reassured by this knowledge.
Obsessions that people commonly have include:
- Fears of contamination or getting dirty
- Fears that they will intentionally or unintentionally harm themselves or others
- Fears of discarding useless or unwanted objects
- Thoughts of blasphemy or being punished for their sins
- Fears of committing unwanted sexual acts
- A need for symmetry or exactness
Compulsions are repetitive behaviors or mental acts performed in an attempt to neutralize the distress or anxiety caused by the obsession Compulsions may or may not be logically related to the obsession. For example, a person with contamination fears may wash repetitively or with a complex routine in order to avoid getting sick or dirty. The same person may also open and close the refrigerator a certain number of times before taking food out to avoid contaminating it. Much like obsessions, the person often knows that the compulsions are excessive or unreasonable, however still feels the need to perform them.
Treatment
Exposure and response prevention therapy (ERP) is a form of cognitive-behavioral therapy that has been shown to be highly effective in treating OCD.
Separation Anxiety
Separation anxiety begins in childhood and is characterized by excessive anxiety related to separation from home or from loved ones (parents, siblings, significant others). This anxiety interferes with social, school, or work functioning. Children and adults who experience separation anxiety often experience at least three or more of the following:
- Recurrent distress when separated from home or attachment figure or when separation is anticipated.
- Excessive worry about losing or harm coming to attachment figure.
- Persistent and excessive worry that an event will lead to separation from attachment figure, for example getting lost or being kidnapped.
- Persistent reluctance or refusal to go to school or elsewhere because of fear of separation.
- Persistent or excessive fear or reluctance to be alone without major attachment figures at home or in other settings.
- Persistence reluctance or refusal to go to sleep without being near a major attachment figure or to sleep away from home.
- Repeated nightmares involving the theme of separation.
- Repeated complaints about physical symptoms such as headaches, stomachaches, nausea, or vomiting, when separation from major attachment figure occurs or is anticipated.
Separation anxiety disorder is not to be confused with normal separation anxiety that occurs in infants and toddlers once they realize that they are separate from their primary caregivers. This normally occurs in children aged 7-14 months old and is sometimes referred to as stranger anxiety.
Insomnia
Insomnia is defined by difficulty falling asleep, staying asleep, or early morning wakening. It is a common problem, with half of adults experiencing it in their lifetime. It negatively affects mood, work and relationships and can become a vicious cycle where the person dreads going to bed at night, making falling asleep even more difficult. There is cognitive-behavioral therapy for insomnia that uses a step-by-step approach proven to improve your sleep without the use of medication. This treatment includes:
- using relaxation and stress reduction techniques
- teaching you to quiet your mind and body
- establishing behavioral techniques that dramatically improve sleep
Depression
Depression is one of the most common mental health problems that affect children, teenagers and adults. Twenty to twenty five percent of people may suffer from major depression at some point in their life. Common causes of depression are: grief or losing a loved one, major life changes, and isolation. Some common symptoms of depression are:
- Sense of hopelessness, despair, worthlessness or guilt (in children or teenagers this may appear as irritability)
- Difficulty concentrating
- Changes in eating and/or sleeping habits
- Fatigue or loss of energy
- Decreased interest or pleasure in activities
- Recurring thoughts of death or suicide
Treatment
Cognitive-Behavioral Therapy consists of helping the person participate in positive daily activities to combat lack of motivation. Therapy for depression also focuses on negative thoughts that are very common in depression. Understanding that these thoughts may not be 100% accurate and developing more realistic ways of thinking can help to alleviate symptoms and deal with depression.
Tinnitus
Are you hearing ringing, hissing, or buzzing in your ears? If so, you may be suffering from tinnitus, a condition characterized by persistent ringing, whistling, buzzing, hissing, or pulsing in either one or both ears, and is usually accompanied by hearing loss. These sounds may come and go for an individual or continually occur, 24 hours a day, seven days a week.
Tinnitus can range from slight annoyance to severe disruption of everyday life and cause significant stress such as:
- Irritability, anger and frustration
- Difficulty sleeping
- Decreased enjoyment of life and withdrawing from activities
- Increased worry or anxiety
The causes of tinnitus vary for each individual. Some of the causes include the following:
- Noise-induced hearing loss and nerve damage
- Earwax buildup
- Prescription and over-the-counter medications
- Rupture of the eardrum
- Ear infection
- Trauma to the neck and head
- Cardiovascular problems, such as hypertension
Getting Help
Due to the personal and unique nature of each tinnitus condition, proper evaluation and treatment is necessary. If you have not already been evaluated by an audiologist, this should be your first step before beginning Cognitive-Behavioral Therapy. Once you and your audiologist have explored the medical treatment options for your tinnitus, (CBT) can help you learn specific tools and strategies to reduce the impact of tinnitus on your daily life such as:
- Relaxation techniques
- Changing how you respond to tinnitus
- Identifying and changing negative thinking patterns
- Training your attention to focus on things that are important to you while reducing the interference of tinnitus.
CBT is a brief approach that has been proven to help improve the quality of life for those suffering from tinnitus.
Trichotillomania/ Compulsive Hair Pulling
Pulling or plucking hair is often a part of normal grooming behavior. However for some people this normal behavior seems to take on a life of its own, becoming an uncontrollable impulse, and can cause many problems for the person including bald spots or thinning of the hair as well as feelings of guilt and shame. CBT can help you understand why this happens and how to stop pulling hair successfully.
Trichotillomania (Trich) is characterized by repeatedly pulling hair from any site on the body (scalp, eye lashes/brows, pubic, arms, legs, etc.) to the extent that noticeable bald spots or thinning of the hair develops. Some people describe a feeling of building tension in their body that is relieved by the pulling, however this is not the case for all people who pull. For some people, pulling is more about the sensory experience than it is about their emotional state before the pulling. Trich often starts during childhood usually around the age of 7-11 years old, though some parents report their child was focused on hair (touching, playing, pulling) long before the pulling began.
Types of Pulling
There are two different types of pulling: focused and automatic.
Focused pulling is used to describe pulling that the person is actively aware of. In these situations the person feels a strong urge to pull that they then consciously act on. These urges can be triggered by a variety of things including environment, emotions, or specific behaviors.
Automatic pulling identifies pulling that takes place outside the person’s immediate awareness. In these situations people often do not realize they are pulling until something/someone brings their attention to it.
Although some people experience only one or the other, a large number of people engage in both types of pulling.
Rituals and Routines
Pulling for many people often involves rituals or routines related to how they pick hairs to be pulled, how they pull the hair, and what they do with the hair once it has been pulled. Some people look for certain types of hair to pull. The selection may be related to the color, texture, or length of the hair. Other times it may be based on the hair looking “out of place” or “wrong”. Once a hair has been selected, some people also have specific ways they pull the hair including using certain fingers or a particular motion. Others may even use things to aid them in their pulling such as mirrors or tweezers. In addition to the routines and rituals related to pulling, there are many different things that people do with the hair once they have pulled it, ranging from discarding the hair in various ways, playing with it, and/or chewing or swallowing the hair or hair root. Although most of these rituals do not have any serious health side effects, swallowing the hair can lead to a build-up of hair that can eventually cause blockage in the intestinal system.
Treatment
The Trichotillomania Learning Center has identified CBT as the treatment of choice for people struggling with Trich. When using CBT, you and your therapist begin by identify the triggers for your pulling as well as what things perpetuate the pulling in order to help you develop specific tools and strategies to more effectively intervene and stop pulling behaviors.
Chronic Skin Picking
Picking or scratching at blemishes or unwanted bumps on your body can be a normal part of daily grooming behaviors. However, for some people this behavior can become excessive to the point that scabbing, skin discoloration, scarring, and even infections can develop. Chronic Skin Picking (CSP), is when a person repeatedly touches, rubs, scratches, bites, or picks at the skin. People may pick at the skin anywhere on the body; however, some of the more common places that people pick are the face, arms, hands, and fingers including the cuticle bed and nails. People with CSP do not wish to cause themselves pain or harm in any way. Instead, they often report their picking as a pleasurable or satisfying activity that can result in long periods of picking without the person realizing the negative impact they are having on their appearance. Because of this, many people with CSP have mixed feelings about their behavior. On the one hand it can feel very satisfying to successfully pick a blemish or bump that was bothersome. However, the negative impact on their appearance and what others think of them often causes feelings of shame and embarrassment about the behavior afterward.
Why Can’t I Just Stop?
CSP can be very frustrating not only to the person who is picking, but to family members and loved ones who do not understand why the person cannot “just stop picking.” Learning to stop is more than just a game of will power, because the picking is more complex than just a bad habit.
Because this is often hard for others to understand, parents of children or adolescents who pick may resort to punishing their child whenever they pick. Unfortunately, this is rarely effective because CSP is not a willful or defiant behavior.
Learning How to Stop Picking
Research has shown that Cognitive Behavioral Therapy (CBT) is one of the most successful ways to help people learn how to stop picking. CBT starts by helping you understand the emotional and physical triggers, situational factors, and associated behaviors involved in the picking. After understanding those triggers, alternative coping strategies are taught to each person with their triggers kept in mind, therefore not every person will benefit from the same coping strategies. These strategies are meant to provide competing motor responses that will direct you away from picking or strategies to help you cope with emotional triggers more effectively. An example could be having something to occupy your hands with such as a rubber ball or small fidget toy during times when urges to pick are higher. If you tend to have more emotional triggers for your picking, then the strategies might involve learning how to more accurately identify your feelings and what to do to help you process them more effectively.
For some people, modifying the physical aspects of your surroundings helps to reduce the urge to pick. For example, by covering mirrors in bathrooms or other high picking areas, you can prevent yourself from looking closely at your face and finding the imperfections to pick at.
Determining the reasons for each person’s picking is an essential part of helping find strategies best suited for that person. When working with children or adolescents who are picking, parents are heavily involved in the therapy to help them understand their child’s behaviors. This helps provide parents with support and feedback on how they can best help their child in learning how to stop picking.

Contact